Minimally Invasive nerve excision

Irritation of the median or lateral branch nerves by enlarged or worn out facet joints of the spine can often cause chronic pain of the cervical, thoracic, lumbar, or sacral regions.
In this case, your doctor may perform a minimally invasive nerve excision, sometimes called a nerve ablation, neurotomy, rhizotomy or avulsion of the medial branch or lateral branch nerves to the facet joints . This procedure offers:
- Fast Recovery
- Less postoperative pain
- Small incision
- Minimal bleeding
- Same day, outpatient procedure
- Most procedures do not require general anesthesia
How it Works
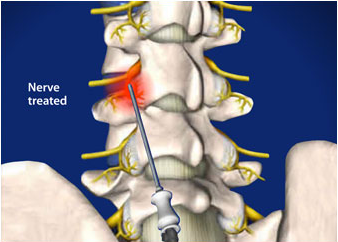
Endoscopic Assisted Nerve Excision may be performed on the cervical (upper), thoracic (middle), lumbar (lower back) or sacral (pelvic) spine areas.
The procedure treats pain associated with facet joints of the spine or other innervated structures. It is performed via minimally invasive surgical technique with the use of a direct visualization device called endoscope or arthroscope.
About the Procedure
During this procedure, an endoscope is inserted percutaneously to the ‘target’ structure and the pain generating nerves, typically a medial branch nerve of the facet joint capsule identified with direct visualization. The endoscope has a working channel through which additional special instruments such as a laser or radiofrequency probe can be inserted. Using these instruments, the pain generating nerves are removed (avulsed and the nerve twigs are ablated) under direct visualization. This process interrupts the pain impulses running up and down the targeted nerve, stopping the pain impulses felt in the area. There is no motor function associated with these pain generating nerves.
What kind of pain does it treat?
The most useful applications for this treatment are for neck, mid, low back, and sacral area pain. Prior to performing nerve excision treatment, a patient is tested by having an injection of a local anesthetic numbing medication into the same location. If there is relief of pain for just a few hours, it confirms the location of the pain site.
Does it hurt?
This procedure is performed with local anesthesia medication to the targeted anatomic area and intravenous sedation medication(s) to relax you during the procedure, so only a slight pressure and minimal discomfort would be felt.
How long does it take?
It takes about 30 minutes per nerve. Typically most patients require ablation of 2-3 nerves on each side. Your length of time in procedure is determined by how many locations are treated.
What can I expect in healing time?
Initially you might have some irritation in the area with some local swelling immediately following procedure. This is a normal reaction to the treatment performed. Ice and anti-inflammatory medications (such as Advil or Aleve) would help. These symptoms might persist for 4-6 weeks. The incisions are tiny hence scarring is often not seen at all after 2-4 months. You may return to work within days, but please discuss this with your surgeon first.
Is it permanent?
Endoscopically assisted nerve excision is a relatively new procedure; hence there are very few published clinical outcomes. All patients at the Spine Institute NW are encouraged to register with the UW Pain Medicine established clinical outcomes database, C-PAIN. Procedure outcomes are also measured using our internal research database. The initial results are quite encouraging and very promising for long term benefit.
What are my risks?
Endoscopic Assisted Nerve excision surgery is a minimally invasive procedure; however as with any surgical procedure there are risks of infection and bleeding. Other risks include swelling of the area, bruising, and incision pain after procedure, and/or loss of sensation to the wrong nerve. Careful steps are taken in all of these areas to minimize risks and maximize efficacy of treatment.
What can I do to prepare?
The nursing staff performs pre-operative evaluation and interviews all of our patients in preparation for the procedure, so all patients will get a chance to have any specifics questions regarding preparation of surgery answered.
Patients are recommended to wear comfortable clothing to the surgery center. You must have a driver to take you home after the procedure. No food or drink six hours before the test. You may take your regular medications with water until 6 hours prior to procedure unless you are specifically directed otherwise by our staff.
What are the differences between Needle Radiofrequency and Direct Visualization Nerve excision?
Needle radiofrequency neurotomy treatment is a percutaneous radiofrequency burning of the nerve via insertion of a needle with a probe that releases heat at its tip. This procedure is done with X-ray assistance and the treatment is applied to the area where the nerve is presumed to be located based on anatomical relationships and with nerve stimulation as guide to proximity. However, because direct visualization of the nerve is not performed and the area treated is small, pain relief is also often short lived.
Direct visualization with an endoscope instrument coupled with X-ray guidance, as done with endoscopic assisted nerve excision surgery, is more precise and can be performed with a greater chance of success and potential reduced recurrence.