INTRODUCTION:
This revolutionary procedure is unlike any previous spine surgery (such as laminectomy or fusion). Using a needle guide with and endoscope under local anesthesia, the damaged disc is visualized under magnification and repaired from the inside. Damaged tissue sections and loose fragments are removed. Using Laser and Radiofrequency (RF) to create shrinkage, the bulging disc segment is pulled back into its original position while creating a stronger lining. Endoscopic microdiscectomy is different from other surgeries in that adjacent muscle and tissue damage is minimized and your anatomy remains intact.
This procedure was invented in the early 1950′s. There are over 30,000 published case reports. In recent times, new technology with laser and RF, in combination with improved optics, has given us minimally invasive access to segments of disc that were not previously considered for surgery. This enabled us to have more access to visualize segments of disc that were either not previously considered or were approached using much more invasive open spine surgeries. This is a curative and restorative procedure for cervical, thoracic and lumbar spine.
PATIENT INFORMATION:
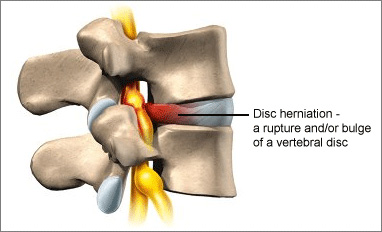
Endoscopically Assisted Spinal Decompression (ED): The selective removal of targeted portions of a bulging disc. This procedure is only performed if the disc is the major source of the patient’s back, neck, leg, or arm pain.
Discoplasty (Nucleoplasty and/or Annuloplasty): Repair of disc damage procedure. It can be achieved by shrinking the inner or outer portions of the intervertebral disc using various techniques such as radiofrequency, coblation, ultrasound, heat (electro-thermal energy), or laser. This shrinks and tightens the disc, which in turn causes the herniation to recede and stop compressing on the nerve. This starts the healing process of an annular tear.
Procedure:
Time in actual surgery is about 90 minutes per disc. Intravenous sedation and local anesthetic will be provided. Using fluoroscopy (an advanced form of x-ray that takes still as well as moving x-ray pictures), an entry is made approximately 10 centimeters from the spine. An arthroscope (also called an endoscope) is passed through the incision, subcutaneous tissue and muscle. At the disc, careful entry is made into the interior of the disc, and disc material is manually removed at the site of the herniation. A radio frequency electrode and YAG: Holmium laser is used to control any bleeding, shrink the inner disc tissue, and shrink the annulus (outside rim of the disc). Occasionally, entry is made from both sides of the spine if indicated.
Expected Results:
The ultimate goal is relief from back, neck, leg, or neck pain. After surgery there will be some discomfort in the surgical area. You will be released to home after about an hour of recovery, and will follow up within one week with Dr. Kamson in the office for suture removal and wound care. Follow up with Dr. Kamson is usually 1-4 weeks. Please remain on bed rest until that time. Physical therapy begins at 4-6 weeks. Return to work varies according to patient response and the type of job they do. Occasionally, you will be placed on “light duty” for the initial return to work and increased to “full duty” as tolerated. Your disc begins to heal at about six weeks! Don’t rush getting “back into the swing!”
Back/leg or neck/arm pain may disappear immediately, but may also take up to several months to quiet down. The pain may change in character or increase in severity. This is a normal reaction. Please be patient and remind your family/friends to “hang in there” as you heal from your procedure.
Risks include infection, injury to the local nerves, unusual nerve sensations, continued pain, disc tears and local muscle bruising. Segmental instability (unstable backbone) may require additional surgery to repair. Scar tissue is minimal with this procedure. This is a “band-aid” type procedure with ¼ inch cut to the skin. Scars are very small.
